Study Rationale
Pediatric organ transplantation poses significant challenges due to varying responses to treatment and the genetic factors influencing outcomes. The rarity of cases limits available genomic data, but integrating data from six European TransplantChild ERN hospitals could contribute to addressing these challenges. The study focuses on liver and kidney transplants, with liver diseases often lacking diagnostic biomarkers and kidney disorders presenting highly heterogeneous phenotypes and genotypes. These complexities complicate early diagnosis and personalized treatment. This study aims to refine diagnostic precision, explore novel therapeutic strategies, and improve outcomes for pediatric transplant patients.
Extent and Evaluation of Current Knowledge
Pediatric transplantation requires lifelong immunosuppression (IS), presenting unique challenges due to children’s metabolic and immune immaturity. Current IS regimens have reduced rejection and mortality but demand tailored approaches to minimize risks like infections, toxicity, and cancer. Genetic factors influencing rejection, allograft failure, and IS complications remain underexplored. This study integrates clinical and genomic data, focusing on:
Epigenetics, particularly DNA methylation, offers potential biomarkers for immune responses, graft injury, and fibrosis, enabling personalized care and improved outcomes.
Objectives of the Study
The study aims to demonstrate the added value of integrating real-world data with genomic markers to predict adverse outcomes in pediatric liver and kidney transplant patients. A pilot study of 200 genomes and methylomes (retrospective and prospective) will analyze genomic and epigenomic determinants to achieve the following goals:
Primary Objectives
Secondary Objective
Integrate genomic data into the Beyond 1 Million Genomes project (B1MG) to support broader research efforts.
Study Design
The clinical study involves two cohorts of pediatric patients with renal or liver transplants from ERN-TransplantChild reference centers. Key steps include:
1. Informed Consent and Recruitment
Patients/families will provide consent for genomic and methylomic analyses.
2. Data Collection and Follow-Up
Clinical data, including adverse outcomes such as infections, rejection episodes, diabetes, and hypertension, will be collected before inclusion and during a 3-year follow-up.
3. Genomic and Methylomic Analysis
Genetic and methylation markers predicting outcomes like infections and rejection will be identified. Episignatures derived from DNA methylation patterns will serve diagnostic purposes.
4. Control Groups
Data from international databases and internal controls (800+ samples) will be used for comparison.
Data integration and mining will link phenotypes to diagnoses and outcomes.
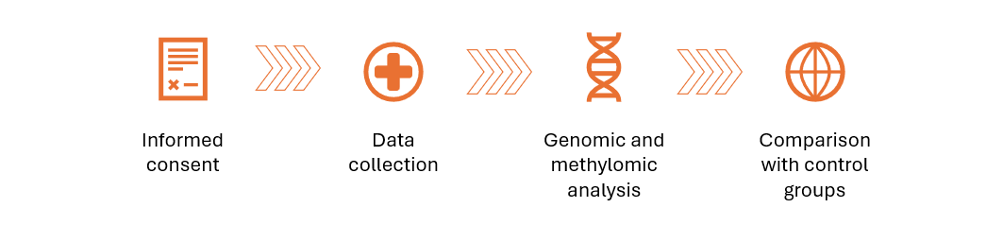
Figure 1. Diagram illustrating the Clinical Study Design, highlighting key steps: informed consent, data collection, genomic and methylomic analysis, and comparison with control groups.
Study Procedures
Part A: Whole Genome Sequencing (WGS) and B-PRS calculation
WGS
Bayesian Polygenic Risk Score (B-PRS) Development
This innovative approach incorporates rare variants and models gene-gene/environment interactions through advanced machine learning.
Part B: Methylomes and Episignatures
Refinement of Episignatures
Discovery and Validation of New Epigenetic Markers
The activity will be aimed at improving the effectiveness of the episignature in liver and kidney transplanted patients.
Anticipated Impact
This study represents a significant advancement in pediatric transplant medicine. By integrating genomic, epigenomic and clinical data, it addresses gaps in diagnostic precision and personalized care. The findings will contribute to developing improved polygenic risk scores, refining episignatures, and paving the way for precision diagnostics and therapeutic strategies. The approach will enhance long-term outcomes and quality of life for children and families navigating the complexities of transplantation.
Top 5 Key Points
1. Collaborative approach for pediatric transplants
Integrating genomic and clinical data from six European TransplantChild ERN hospitals addresses the scarcity of data and diverse responses in pediatric liver and kidney transplants.
2. Focus on Genomics and Epigenetics
Utilizing Whole Genome Sequencing (WGS) and DNA methylation analysis (episignatures) to identify markers for organ rejection, infection susceptibility, and disease-specific traits.
3. Innovative risk assessment with B-PRS
Development of Bayesian Polygenic Risk Scores, incorporating rare variants and machine learning, to improve predictive accuracy for adverse outcomes in transplant patients.
4. Refinement of episignatures
Enhancing diagnostic specificity and sensitivity by analyzing at least 200 patients, leveraging federated learning to ensure secure data refinement without compromising privacy.
5. Impact on personalized medicine
Establishing precision diagnostics and therapeutic strategies to improve long-term outcomes and quality of life for pediatric transplant patients and their families.

This project has received funding from the European Union’s Horizon Europe research and innovation programme under grant agreement Nº 101137423, as well as the Swiss State Secretariat for Education, Research and Innovation (SERI).